 Peer Support Services in Crisis Care
Peer Support Services in Crisis Care
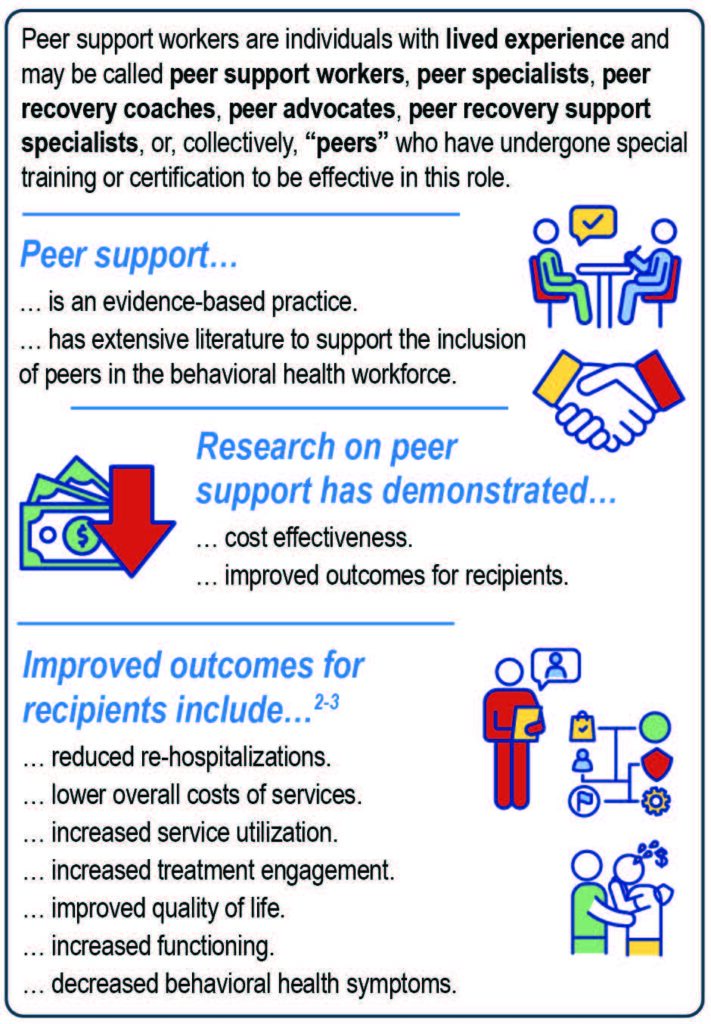
Peer support workers—also known as peers—are individuals with lived experience who have sustained recovery from a mental or substance use disorder, or both.1 They assist others entering or in recovery with reducing the recurrence of symptoms, more commonly known as relapse.2-4 Peers model recovery, promote shared understanding, focus on strengths, offer positive coping strategies, and provide information and resources.1
Peers may engage in a range of non-clinical activities to support individuals or families of individuals in or seeking recovery from a substance use disorder, mental illness, or both. Activities may include mentoring, advocating for people in recovery, leading recovery groups, and building relationships.1 These activities supplement other services an individual may receive. The role of the peer is unique in that it is based on the concept of mutuality—or sharing similar experiences. Peers offer a non-hierarchical relationship that differs from individuals’ relationships with clinicians. Peers enhance the work of an individual’s clinical care team and support them and their families as they navigate recovery.2, 4
Key Messages
- Peer support services are an integral component of the behavioral health continuum of care—from prevention and early intervention to treatment, recovery, and crisis services.
- Crisis care provides services to anyone, anywhere, at any time. Three essential elements comprise crisis care: crisis phone lines, mobile crisis teams, and crisis receiving and stabilization facilities.
- There are several benefits to including peers in crisis care, including strengthening engagement in treatment and improving outcomes for individuals experiencing a crisis who receive these services.
- Peers working in crisis service care settings provide opportunities for individuals in crisis to talk with someone who has similar experiences, embodies recovery, and can offer messages of encouragement and hope.
- Peers may experience challenges related to role integrity, stigma from co-workers, and sustainable employment. They also face challenges unique to providing crisis care, including the complexity of managing crisis situations and, often, a lack of specialized crisis training.
Definitions
Behavioral health:5 A key part of a person’s overall health, which includes emotional, psychological, and social well-being, and that is just as important as physical health. Conditions that may impact behavioral health include mental illnesses, substance use disorders, and co-occurring mental and substance use disorders.
Behavioral health continuum of care:6 An integrated system of care with varying levels of service intensity and settings in response to an individual’s behavioral health needs.
Crisis care: 7 A range of services for individuals experiencing an acute mental and/or substance use disorder crisis.
Crisis respite:7 Short-term, residential facilities that offer a restful, step-down environment with supports for individuals experiencing a crisis.
Lived experience:2 Personal knowledge gained through direct, first-hand involvement.
Mutuality:2 A positive, interactive relationship between people based on shared lived experience.
Peer drift:8 When the role of the peer support worker begins to deviate from the practices that distinguish peer support workers from clinical providers or other recovery supports.
Peer support services:2 Peer support services encompass a range of activities and interactions between people who share similar experiences of being diagnosed with mental health conditions, substance use disorders, or both.
Peer support workers:1 People who have been successful in the recovery process who help others experiencing similar situations. Through shared understanding, respect, and mutual empowerment, peer support workers help people enter and stay engaged in the recovery process and reduce the likelihood of relapse. Peer support workers are trained as recovery coaches or peer specialists and may include family peer supporters.
Recovery:9 A process of change through which people improve their health and wellness, live self-directed lives, and strive to reach their full potential. The four dimensions that support recovery are health, housing, purpose, and community.
Recovery capital:10 The internal and external resources that are available to individuals to initiate and sustain recovery from mental and/or substance use disorders.
Recovery support services:9 A range of non-clinical support services designed to help people with mental and substance use disorders manage their conditions successfully.
Recurrence of symptoms:11 A phase of recovery where a person’s symptoms have returned and their functioning has decreased. This may be more commonly referred to as “relapse.”
Strengths-based:12 An approach to assessment and care that emphasizes the strengths of the individual.
Trauma-informed:13 Services or care based on the knowledge and understanding of trauma and its far-reaching implications.
Warm line:7 A phone line individuals can call to receive services that are less intensive than what one would receive when calling a hot line, like opportunities for talking, support, and referrals to other services.